Abstract
Background: Use of direct-acting oral anticoagulants (DOACs) in morbidly obese (BMI >40 kg/m2) patients for venous thromboembolism (VTE) treatment is not fully understood. Current International Society of Thrombosis and Haemostasis guidelines do not recommend DOAC use in morbidly obese patients due to limited clinical data in this patient population.
Objective: Compare risk of recurrent VTE, major bleeding, healthcare resource utilization, and costs between morbidly obese VTE patients initiating rivaroxaban or warfarin treatment.
Methods: This is a retrospective 1:1 propensity score matched cohort study. VTE patients initiating rivaroxaban or warfarin were identified from Truven MarketScan Commercial Claims and Encounters and Medicare Supplemental database (12/1/2011-12/31/2016). An ICD-9/ICD-10 diagnosis code for morbid obesity was required during the 12 months pre- or 3 months post-initiation. Patients were followed ≥3 months. Analyses were conducted during the entire follow-up period regardless of discontinuation as well as on-treatment prior to discontinuation of index treatment. Major bleeding was assessed using the validated claims-based algorithm developed by Cunningham et al. 2011. Conditional logistic regression and generalized linear models were used to compare recurrent VTE and major bleeding risks, all-cause healthcare resource utilization, and per patient per year (PPPY) costs.
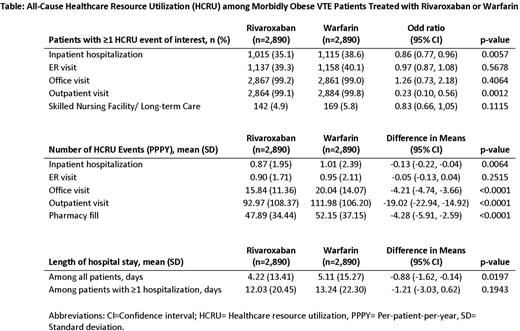
Results: Among 5,780 rivaroxaban or warfarin treated patients (2,890 in each matched cohort), mean age was 53 ±13 years; 60% were female; mean follow-up time was 10.0 months and 10.5 months, respectively. Mean time between VTE diagnosis and treatment start was 14 days. Risk of recurrent VTE was similar for both cohorts in the intent-to-treat analysis (OR: 0.99, 95% CI: 0.85-1.14, p=0.844). Major bleeding risk was numerically lower for the rivaroxaban cohort but did not reach statistical significance in the on-treatment analysis (OR: 0.75, 95% CI: 0.47-1.19, p=0.227). Rivaroxaban treated patients utilized fewer all-cause healthcare resources, specifically inpatient hospitalizations (OR: 0.86, 95% CI: 0.77-0.96, p=0.006) and outpatient visits (OR: 0.23, 95% CI: 0.10-0.56, p=0.001) compared to warfarin (Table). Rivaroxaban patients incurred an average $2,829 lower total medical costs PPPY, ($34,824 vs $37,653, p=0.020), mainly driven by hospitalization costs. Total healthcare costs (including pharmacy) showed a numerical $1,531 reduction for rivaroxaban patients, not reaching statistical significance ($43,034 vs. $44,565, p=0.237).
Conclusions: Our study showed that morbidly obese VTE patients treated with rivaroxaban had similar risk of recurrent VTE and major bleeding compared to warfarin. Treatment with rivaroxaban yielded less all-cause healthcare resource utilization (i.e. inpatient hospitalizations and outpatient visits) and reduced total medical costs.
Spyropoulos:Janssen Scientific Affairs, LLC: Consultancy. Ashton:Janssen Scientific Affairs, LLC: Employment. Chen:Janssen Scientific Affairs, LLC: Employment. Wu:Janssen Scientific Affairs, LLC: Employment. Peterson:Janssen Scientific Affairs, LLC: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal